 According to the National Institutes of Health, more than eighty percent of children will get an ear infection by age three,1 which is unpleasant for children and parents alike. Severe ear infections can even lead to permanent hearing loss. Despite their regularity, these infections can be a real pain in the ear to diagnose and cure. Luckily, new technology being developed by department of bioengineering researcher Alexander Ho has the potential to improve the diagnostic process and speed up delivery of the correct treatment. The work is so promising that it has been awarded the McGinnis Medical Innovation Graduate Fellowship, an award funded by a generous gift from the late Illinois alumnus Jerry McGinnis.
According to the National Institutes of Health, more than eighty percent of children will get an ear infection by age three,1 which is unpleasant for children and parents alike. Severe ear infections can even lead to permanent hearing loss. Despite their regularity, these infections can be a real pain in the ear to diagnose and cure. Luckily, new technology being developed by department of bioengineering researcher Alexander Ho has the potential to improve the diagnostic process and speed up delivery of the correct treatment. The work is so promising that it has been awarded the McGinnis Medical Innovation Graduate Fellowship, an award funded by a generous gift from the late Illinois alumnus Jerry McGinnis.
A major reason ear infections can be so difficult to treat is due to where in the ear an infection manifests. Ear infections build in strength and severity in the middle ear, which is hidden behind the eardrum. Doctors can’t see it well when they’re doing diagnostics. Worse yet, biofilms- bacterial structures that are resistant to treatment- can form in the back of the ear, wreaking havoc while remaining out of sight.

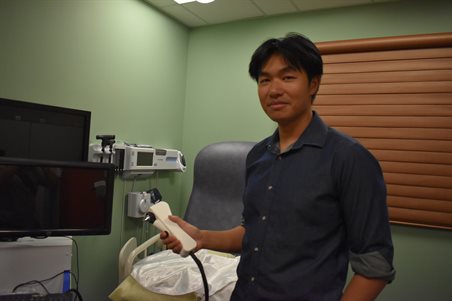
The solution, Ho says, is combining a few revolutionary techniques into one handheld device that can look behind the eardrum, where the heart of the infection is. These technologies are called Optical Coherence Tomography (OCT) and Raman spectroscopy.
OCT can take a picture of hidden tissue to look at the structures that are out of sight. “If you’re familiar with ultrasound, it’s essentially the same concept,” says Ho. “With ultrasound, sound waves are sent in and we measure the time it takes for the sound to bounce back. We can turn that information into a picture. We try to do the same thing with OCT, but with light.” This would allow the doctor to see behind the eardrum to reveal any infections, fluid build ups, biofilms that may be hiding.
While OCT reveals structure, Raman spectroscopy can see the chemical content of what lies beyond the outer eardrum. Ho explains: “Just like everyone has a unique fingerprint, molecules have their own unique ‘fingerprints’ too. To see these fingerprints, we shine a laser on the molecules and measure the light that comes back.” This would reveal exactly what species of bacteria was causing the infection and enable physicians to choose more effective treatments.
The team is currently building probes for patient imaging at Carle, which will be ready around the fall. Within the next year they hope to test ten patients and build machine learning models for analysis. From there, they hope to launch a larger study with Carle.
 Ho went out of his way to point out the exceptional support around him. “It’s not just me on this project. I get a lot of help from everyone: Dr. Guillermo Monroy, Edita Aksamitiene, Darold R. Spillman, Sean Fitzgerald, Alec Walter, Christine Canfield, Prof. Anita Mahadevan-Jansen, and of course Dr. Stephen Boppart.” In addition, the team is collaborating with professor Anita Mahadeven-Jansen’s lab at Vanderbilt University and Carle Foundation Hospital ENTs Dr. Ryan Porter and Dr. Jonathan McJunkin.
Ho went out of his way to point out the exceptional support around him. “It’s not just me on this project. I get a lot of help from everyone: Dr. Guillermo Monroy, Edita Aksamitiene, Darold R. Spillman, Sean Fitzgerald, Alec Walter, Christine Canfield, Prof. Anita Mahadevan-Jansen, and of course Dr. Stephen Boppart.” In addition, the team is collaborating with professor Anita Mahadeven-Jansen’s lab at Vanderbilt University and Carle Foundation Hospital ENTs Dr. Ryan Porter and Dr. Jonathan McJunkin.
There are many challenges ahead- in addition to testing, the team also wants to shrink the spectrometer to about half the size it is now to make it easier to use on young children. But the future is bright, and we’re all excited to see where this technology can go from here.
1https://www.nidcd.nih.gov/health/ear-infections-children#:~:text=Anyone%20can%20get%20an%20ear,is%20otitis%20media%20(OM).